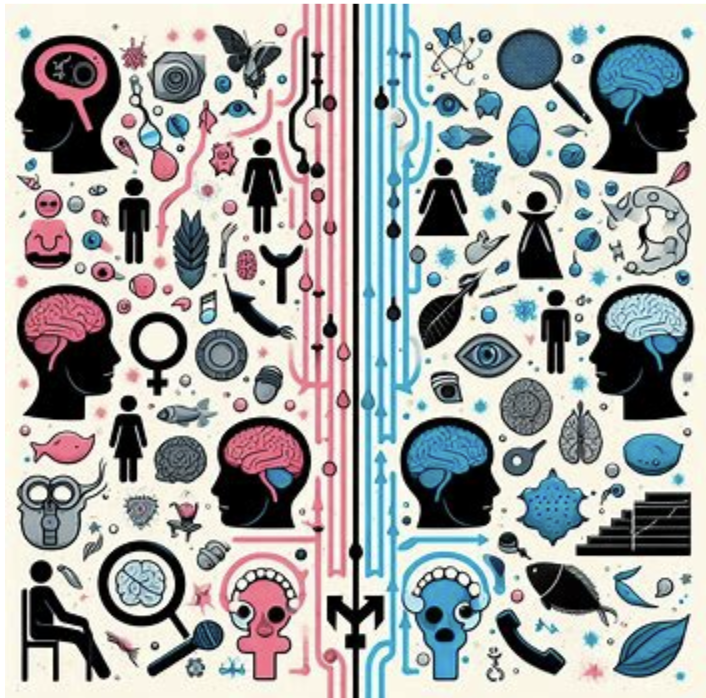
That’s a rhetorical question of course, but it highlights an issue that has pervaded medical disease research for decades if not centuries and remains disturbingly persistent in the process of treatment today. The following article is a long read, yet it can only scratch the surface of the topic, which despite relatively recent improvements, remains heavily biased and requires a great deal of nuance and patience to address. Discussions about biological sex are a challenge on many levels, and the dire lack of substantial research on trans and intersex participants has meant that I have had to narrow the scope of this article to focus on cisgender participants.
If you undertook any form of scientific education that involved a section on evaluating research and articles in journals, you may have been informed that in much of medical literature, there is less information specific to women outside of reproductive systems. You may have been told about the rather infamous update within the medical community that had to inform everyone that women do not, in fact, respond to cardiovascular disease in the exact same way as men do. This highlighted a problem that pervades much of medical science, namely that most clinical research and medical observations are based upon men. Given the apparent differences in biological systems present between men and women, one would have assumed that sex is a factor that has always been taken into consideration for clinical treatment studies. However, it was not until 2014 that the United States National Institute of Health, one of the foremost research regulators and funding bodies in the world, decreed that preclinical trials must show that sex was a considered variable when applying for funding. Naturally, many similar institutes around the world have followed suit, but the fact that this occurred as late as 2014, when preclinical trials on psychiatric disorder treatments had already been persisting for decades, is alarming to say the least.
The ramifications of lax policies around the representation of separate sexes in trials are numerous, as the lack of knowledge and attention has the potential to not only lead to inadequate treatment in women, but may also cause bodily harm due to a lack of understanding. One journal article reviewing the topic identified that just over half of the studies looking at disorders known to be prevalent in women actually reported the sex of participants, and of that half, only 12% included either females (lab animals or people) or both sexes. Although this article mostly focuses on women in psychiatric research, the importance of equal gender representation reflects on men. Without accounting for both genders, we would not know that metabolic syndromes such as diabetes are elevated in men, which enables further research into understanding what makes men more at risk. Similarly, there are lessons to be gained from research on psychiatric disorders that disproportionately affect women, which may benefit men as well.
Hormonal steroids are known to play numerous roles across the central nervous system and have resulting impacts on our ability to think (cognition). The role of testosterone in cognition is better understood than the female-centric, gonadal hormones estradiol and progesterone. Despite what sex-ed (or there lack of for some) may have insinuated, men also have levels of estradiol and progesterone, and women have levels of testosterone. Thus, it is important for all sexes to study the roles of these superficially understood gonadal hormones in psychiatric disorders that impact cognition. Such research is not only beneficial to cisgender men and women, but also those transitioning, who through hormone replacement therapy (HRT) could be affecting their risk of developing certain psychiatric disorders, in addition to the intended effects of hormonal therapy. Given the prevalence of the disorders schizophrenia, bipolar disorder and PTSD in both men and women, this has been a good avenue for researchers to investigate.
Schizophrenia
Men develop the disorder almost 1.5x as much as women do, and are less responsive to antipsychotic treatment medications, with women statistically showing higher rates of recovery from the disorder. Schizophrenia presents with numerous symptoms including psychotic (hallucinations and repetitive motion), mood (low energy and motivation), and cognitive (difficulties in learning and paying attention). Some studies have even shown that women with schizophrenia do not display the same structural differences in their brains that men do compared to those without the disorder. However, due to the numerous stages of substantial hormonal landmarks in women’s lives (puberty, pregnancy, post-pregnancy, and menopause), women’s risk of experiencing an onset of schizophrenia can increase, for example during menopause. The differences in rates between sexes and the risk of second onset has led to the so-called “estrogen hypothesis” in psychiatric research that posits a protective role that the family of hormones “estrogens” may play against schizophrenia development and severity. Observational evidence for this can be seen in the menstrual cycle, where periods of low estradiol (the most common estrogen in the human body) coincide with worsening symptoms. The inverse is also seen in pregnancy, where levels of estradiol and the other gonadal hormone, progesterone, are orders of magnitude higher in the body than before, and symptoms improve over the period. It’s not just women too, both schizophrenic men and women have been shown to overall possess below normal concentrations of both hormones.
Bipolar Disorder
Bipolar disorder (BD) often presents as one of three types, characterized by their fluctuation between extreme highs and lows of mood. Between men and women, BD rates are about equal, although mounting research suggests that a subtype of BD, BD-II is more common in women than men. BD is also a strong example of the importance of treating men and women differently. Women more frequently develop other cognitive disorders alongside the BD, such as PTSD and anxiety, and additionally cannot be treated with the same medication as men, who are less likely to develop hypothyroidism and migraines from lithium, than women. Unlike with schizophrenia, however, it is impossible to make any assertions on the differences in cognitive symptoms and brain structures between men and women, due to a lack of quality research. Despite this, there are studies observing the symptoms of women with BD, which show that not only are women’s menstrual cycles frequently abnormal before they are diagnosed with BD, but symptoms also worsen during periods of lower estradiol, presenting as an increase in manic episodes. Subsequently, transitions from periods of very high hormone levels to very low, such as after pregnancy, can lead to relapses in BD.
PTSD
For this, I would like to start with a direct quote from the article that inspired this piece, which I strongly encourage anyone that wants to know more to read. “One of the most robust risk factors of PTSD is being female.” Women are twice as frequently diagnosed with PTSD as men, and there are naturally many social factors that may contribute to this from increased likelihood of being victim to physical, sexual and verbal abuse, to being more likely to seek diagnosis from a therapist. Nevertheless, even once these social influences had been accounted for in a U.S-wide study of 34000+ participants, women still came above men, suggesting a cause beyond societal influences (although one can only account for social influences to a limited extent). The study highlights that although the symptoms are similar in both sexes, women appear to experience them more intensely than men, perhaps because women also recall the traumatic memories with greater clarity. Women were also reported to more often recall dissociating during the event and feeling that their life was at threat, than men did. Although women are more likely to develop PTSD following traumatic events, women also experience better outcomes from behavioural intervention treatment than men.
Estradiol is a crucial regulator in the process of extinguishing the fear associated with unpleasant memory recall. Research has shown that women with higher estradiol levels in their blood performed better on such tasks in a lab. Indeed, women with lower estradiol and women with PTSD both responded poorly to unpleasant stimuli in a lab. Consequently, there is further indication that estradiol may have a protective effect against fear association with memory. PTSD is where the importance of progesterone finally comes into play (although it may be just as important elsewhere, we just don’t have the research to know). High progesterone levels during specific menstrual phases were seen to actually worsen performance in similar fear-removal tasks, and when both estradiol and progesterone were high, PTSD symptoms tended to worsen. From what research is available, conclusions indicate that progesterone may increase the fear association with memories when they are being encoded after a traumatic event, thus women experience the memories more intensely later in life.
Research, research, research.
We need a lot more of it, period. This does not discount the research that is available from studies on men, as those have proven to be informative and a useful groundwork for treating disorders in all sexes. Yet, when it comes to investigating sex-specific treatments, the studies that are available are inconsistent in methodology, measurement, participant count and ratio of men to women. Lastly, the fact that many of these studies are observing the correlation between hormone levels and symptoms in participants means there is no guarantee that manipulating these systems will lead to the effects showcased above. Consequently, it is incredibly difficult to draw firm conclusions and instead the information above all inspires more and better-quality research.
The menstrual cycle, for example, has not always been considered as a reported variable in clinical studies, nevertheless it presents a unique modality for observing the impact of varying neuro-active hormonal steroid levels in the body. If the importance of high versus low estradiol, progesterone and even testosterone can be understood in how they affect symptoms of psychiatric disorders such as the above, it could lead to improved, better-tailored treatments for everyone. Already one study has tried administering low-dose estradiol along with antipsychotics in men, resulting in improved symptoms and no feminizing side-effects. It is fantastic that modern studies are considering sex as an important variable in clinical research; now we just need to make up the lost ground.
Author: Thomas von Rein
References